Strabismus in children and adults
What is strabismus?
Strabismus is the loss of ocular alignment. This occurs when one of the eyes has deviated and lost coordination with the other. The point of gaze is no longer the same when looking at an object, and the eyes are not aligned anymore. The condition occurs in both children and adults.
It may lead to double vision (diplopia), confused vision and a loss of binocular vision, losing depth perception. Signs may include an abnormal head position (torticollis) or winking one eye to avoid double vision (diplopia).
If strabismus is not diagnosed and treated at an early age, it may lead to sensory alterations such as suppression of the unaligned eye, causing amblyopia (or lazy eye).

5% of children suffer from strabismus.
Causes of Strabismus
Idiopathic: In other words, there is no known cause. This is the most frequent situation.
Accommodative: When a child attempts to accommodate in order to compensate for long sightedness, generally inwards (esotropia).
Anisometropia: The difference in the refraction defect between both eyes leads to the development of strabismus.
Amblyopia: The visual deficit in some types of amblyopia may lead to a lazy eye becoming misaligned over time.
Systemic or neurological muscular paralysis: Paralysis in an extra-ocular muscle due to a neurological condition or systemic diseases that affect muscle innervation may lead to strabismus.
Strabismus composed with horizontal (endotropia) and vertical component (hypotropia).

Strabismus does not always have a concrete cause.
Accommodative esotropia.
Types of strabismus
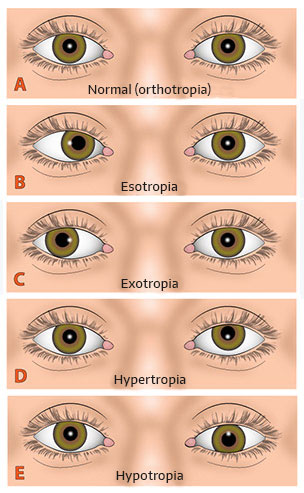
Strabismus is normally classified by the direction of the misalignment.
- Horizontal: This might be a divergent strabismus, where one of the eyes deviates outwards, also known as exotropia. In contrast, convergent strabismus occurs when one of the eyes deviates inwards, also known as esotropia.
- Vertical: When one of the eyes deviates up or down (hypertropia or hypotropia).
- Torsional: When the deviated eye rotates about the eye’s visual axis. This is also known as cyclotropia.
- Combinations of the above: Sometimes there are horizontal, vertical and even torsional misalignments at the same time.
There are other specific types of strabismus, such as Duane syndrome, Brown syndrome, ocular-motor paralysis, nystagmus or fibrosis of the inferior rectus muscle.
Convergent strabismus of the left eye and divergent strabismus of the right eye.
Evaluation
Diagnostic techniques
Cover test
This test objectively determines the presence and amount of ocular deviation. It is used to determine and measure the presence of evident strabismus or tropia, latent strabismus or phoria. It consists of two parts:
The cover-uncover test, in which one eye is continuously covered and uncovered and the movements of both eyes are observed (to measure tropia).
The alternating cover test, in which the eye that is covered is alternated and the movements of the eyes are observed when the other is covered and uncovered (to measure tropia and evaluate phoria).
Technological instruments
Gazelab™ Video-oculograph
GazelabTM video-oculography is based on computer vision technology and projection system put on the patient’s own head. We are then able to achieve objective measurements to study strabismus: ocular movements, nystagmus, pupils and eyelids, with a greater degree of precision than other types of video-oculography.
Gazelab™ is the only system that projects and films from a helmet. This makes testing much easier, and opens up the possibility of examining children (who are unable to sit still for an examination with a chin rest).
Synoptophore
This instrument is used to evaluate and diagnose strabismus. It is also used for visual training and to stimulate lazy eyes (amblyopia). The synoptophore can be used to measure other aspects of vision such as the level of binocular fusion.
Hess Lancaster Screen Test
The Hess Lancaster test (H-L) is a subjective-objective motor evaluation test that examines the extra-ocular muscle function; with one eye being fixated while the other is evaluated. It can help to differentiate paretic strabismus caused by a neurological injury from a motor restriction.
OTHER SPECIALITIES
Related videos
Cases of pre and postoperative strabismus.
Strabismus treatment
For adults
In low-grade deviations or small angles of misalignments, surgery is the most appropriate treatment option, together with glasses, prisms or visual therapy.
Surgery is very effective in terms of aesthetic results.
Accommodative strabismus can only be corrected with glasses or contact lenses. The refractive error causing strabismus may be corrected with refractive surgery, eliminating the strabismus in passing, without the need for surgery.
Adult with convergent strabismus before and after surgery.
For children
Convergent strabismus and hypermetropia can only be optically corrected (glasses or contact lenses). In all other cases, surgery may be required in addition to optical correction. The surgery is simple, but will require a general anaesthesia in the case of children.
If divergent strabismus occurs from birth, we first request a neurological examination, as this type of strabismus may be accompanied by a prior pathology.

Convergent strabismus can be corrected with glasses or contact lenses.
Frequently Asked Questions
If the strabismus has been constant since birth, you should make an appointment as soon as possible; if the misalignment is intermittent, you can visit us from 6-7 months. Early diagnosis of this pathology may avoid learning difficulties and above all, could prevent amblyopia or a lazy eye, as strabismus is the main cause of these conditions. If strabismus appears in adulthood, then neuro-ophthalmological causes must be ruled out.
No. In many cases, strabismus is combined with refractive problems such as hypermetropia. We know that when this occurs early in life, it may lead to convergent strabismus. When hypermetropia is corrected with glasses or lenses, the strabismus partially or even totally disappears. In children, hypermetropia may subside over time or disappear on its own, taking the strabismus with it.
Strabismus surgery is performed on the muscles that move the eyes. The surgical procedure is an operation on the extraocular muscles in charge of ocular motility. Depending on the type and intensity of the deviation, one eye or both are operated. The surgery consists in weakening the most active muscle or muscles, together with strengthening the weakest muscles, if necessary.
Strabismus surgery is usually carried out as an outpatient procedure, causing mild or moderate irritation that is alleviated with common painkillers. Children will require a general anaesthesia.
Nystagmus (or the clinical term opto-kinetic nystagmus) is when an involuntary natural and physiological movement of both eyes occurs when attempting to focus your gaze on a stimulus. In the majority of cases, there is no definite origin and it is present from birth.
When nystagmus is acquired or pathological, it is usually accompanied by a visual acuity deficit and in many cases torticollis (wry neck), towards the point of gaze where the nystagmus is reduced or disappears, known as the block position.
The objective of treating nystagmus is to improve visual comfort, improve visual acuity and minimise torticollis. It is normally treated with glasses, but it may sometimes require surgery. Generally, the characteristics of nystagmus surgery are similar to those of and strabismus surgery.
Sometimes there may appear to be a strabismus where one does not actually exist. This is known as a false strabismus (pseudostrabismus). The two most frequent causes of a false strabismus are: the epicanthal fold, which looks like a convergent strabismus, and hypertelorism, which mimics a divergent strabismus.
Hypertelorism is an exaggerated distance between the eyes, which may give the appearance of an outward strabismus. In the case of the epicanthal fold, one of the eyes may appear to be misaligned because of the nasal fold in some children (vertical, bilateral cutaneous folds extending from the upper or lower eyelids to the inner edge), with an increased perception of misalignment if the said folds are asymmetrical. The epicanthal fold disappears as the child grows and does not require surgery or treatment.
Related entries
What is congenital strabismus?
Before commenting on what congenital strabismus is, keep in mind that strabismus can be classified in relation to several factors:…