Ocular Surface
What is the ocular surface?
An ophthalmological study of the ocular surface includes the prevention and treatment of conditions involving the cornea, conjunctiva and tear film.
The cornea is the transparent layer forming the anterior part of the eye. It protects the remaining layers and focuses light like a lens on the retina so that we can see. It is made up of five layers of tissue, and is covered by a transparent membrane with micro-vessels, called the conjunctiva, which in turn is covered by the tear film.

A healthy ocular surface.
Ocular surface disorders
Corneal degenerations
- Keratoconus: Progressive deformation of the cornea (a lump-like protrusion) in the central and lower side, caused by the cornea thinning (ectasia). The condition causes a progressive increase in refractive error and reduced quality of vision. In advanced cases it can affect corneal transparency.
- Involutional corneal degeneration: This appears naturally or through normal cornea ageing. This is more common at advanced ages, and usually only manifests in one eye without affecting vision.
- Non-involutional corneal degeneration: Not related to ageing, but instead related to metabolic changes. The most common types are band keratopathy (related to calcium deposits) and lipid degeneration (related to fats). They may affect vision.
- Corneal dystrophies: Uncommon genetic diseases that have a severe impact on vision. The most common is Cogan’s dystrophy, which causes discomfort and loss of vision, and Fuchs’ dystrophy, which can be painful.
Conjunctival degeneration
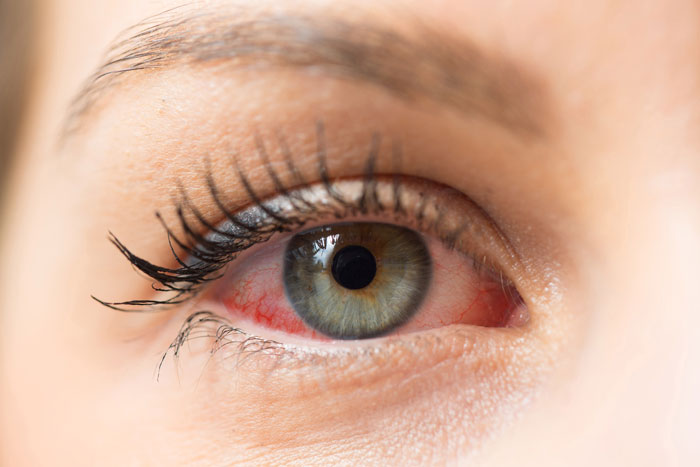
- Pinguecula: An alteration to the conjunctiva in the inner area of the white part of the eye, related to sun exposure. It starts off transparent, then turns white and yellowish with age. It can sometimes become swollen (it looks red) and may be itchy.
- Pterygium: This condition starts out like a pinguecula, but then grows in a comet shape and can invade the cornea, changing its appearance (fleshy and with blood vessels). It is important to treat this condition before it reaches the cornea, as it can deform the cornea and leave a scar.
Detail of the cornea and dry eye effect.
Dry Eye Syndrome
Dry eye is a very common chronic inflammatory condition, suffered by almost one third of the population. The usual symptoms are a sensation of “sand” in the eyes, and other symptoms, such as: burning sensation, heavy eyelids, tired eyes and photophobia (light sensitivity). The causes are of two types: either the eye does not make enough tears, or the tears evaporate too quickly, though the most common cases are mixed. Evaporative dry eye is usually caused by a dysfunction in the Meibomian glands (MG), which are glands in the eyelids whose secretion is essential for the composition of tears.
It is more common in women than men, especially after 50 years of age. Within the risk factors associated to dry eye, we include:
- Environmental factors, such as working with digital screens, continuous exposure to air conditioning, or wearing contact lenses.
- Systemic illnesses, such as Sjögren’s syndrome, rheumatoid arthritis, lupus, diabetes or hyperthyroidism.
- Taking medication for the heart, allergies or high blood pressure, anti-anxiety medication or anti-depressive medication.
Dry eye syndrome usually gets worse with age, and can, in some cases, cause a loss of quality of like which may even be incapacitating. That is why it is important for dry eye to be diagnosed, evaluated and treated by an ophthalmologist specialised in dry eye syndrome.
Evaluation
Diagnostic techniques
Ocular surface examination using a slit lamp, a binocular microscope with different magnification settings and light.
Fluoresceinogram: The eye is stained with fluorescein (a biocompatible dye) before being examined under a blue light. The dye stains the patient’s tear film and corneal lesions.
Schirmer’s Test. This test measures the amount of tears, with strips that rest directly on the eyelid.
Technological instruments
Corneal pachymetry: This measures the thickness of the central cornea.
Corneal topography: An apparatus that measures corneal curvature and surface regularity.
A slit lamp allows the ophthalmologist to determine the position, depth and size of any alteration to the anterior segment of the eye (conjunctiva, cornea, anterior chamber, iris and lens). With the help of special lenses, it is also possible to study the posterior segment (vitreous, retina and optic nerve).
Schirmer’s Test.
OTHER SPECIALITIES
Treatments
Ocular surface
Keratoconus: Treatment is based on four points:
- Glasses or contact lenses: Glasses are used to begin with, but special contact lenses are better later on.
- Cross-linking: The cornea is instilled with a vitamin, riboflavin, to increase its hardness and therefore stop the ectasia. This treatment is applied in the early stages of the disease.
- Intrastromal corneal rings: These are curved rings that are implanted inside the cornea to flatten it. They are recommended for very curved corneas.
- Lamellar transplant (for one part of the cornea) or penetrating transplant (for the whole cornea): In its final stages, the damage will start to form scars that require tissue transplant surgery.
Corneal degeneration does not usually require treatment, and rarely needs surgery or a transplant.
Corneal dystrophies require treatment depending on their seriousness, with treatment normally required for complications. If the condition is serious and advanced, a transplant may be required.
Pinguecula: This condition rarely requires treatment.
Pterygium: In its early stages this condition only requires eye drops or anti-inflammatory drops, but if it grows or almost touches the cornea then surgery will be required. There are two types:
- Simple removal: In 50% of cases the pterygium will reappear, especially in young people.
- Removal followed by a conjunctival graft: After extraction, the area is covered with conjunctiva from the upper area of the same eye. The risk of reappearance is very low (less than 5%) and the result looks better.
Dry Eye Syndrome
Dry eye symptoms are treated using artificial tears of different types. Depending on the degree of dryness in each case, artificial tears of different densities can be used, or even a get to be applied to the yes at night. When artificial tears are not enough, a medication called cyclosporine is used. And in the most severe cases, such as those associated to Sjögren’s syndrome, autogenic serum is used.
The treatment, as such, for dry eye will depend on the cause of the syndrome:
- When it is due to a systemic cause, the treatment of the baseline disease may improve the symptoms, as is the case with diabetes.
- In other cases, the direct cause of dry eye may be found in the eyelids. Eyelid hygiene, using towelettes, often has good results.
- There are other innovative and effective treatments to deal with dry eye syndrome caused by a dysfunction of the Meibomian glands:
- Glandular massage for the Meibomian glands (MG).
- MG catheterisation.
- Application of heat on the MGs.
- IPL laser.


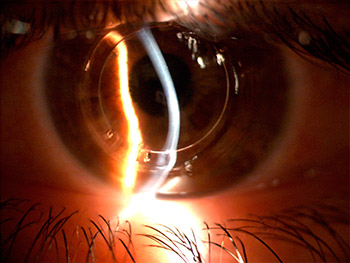
Intrastromal corneal rings.
Related entries
Solar radiation and eye health
Solar radiation affects our eye health more than we can imagine. Solar rays are formed not only by the visible…